Crohn’s and Colitis
WHAT ARE CROHN’S AND COLITIS?
Inflammatory bowel disease (IBD) describes a group of conditions, the two main forms of which are Crohn’s disease and ulcerative colitis. IBD also includes indeterminate colitis.
Crohn’s disease and ulcerative colitis are diseases that inflame the lining of the GI (gastrointestinal) tract and disrupt your body’s ability to digest food, absorb nutrition, and eliminate waste in a healthy manner.
Below you fill find more information about the anatomy and function of the gastrointestinal (GI) tract, Crohn’s disease and ulcerative colitis.
Dr. Mike Evans is founder of the Health Design Lab at the Li Ka Shing Knowledge Institute, an Associate Professor of Family Medicine and Public Health at the University of Toronto, and a staff physician at St. Michael’s Hospital. This video was made possible through the Gastrointestinal Society, with the support of Crohn’s and Colitis Canada.
ANATOMY AND FUNCTION OF THE GI TRACT
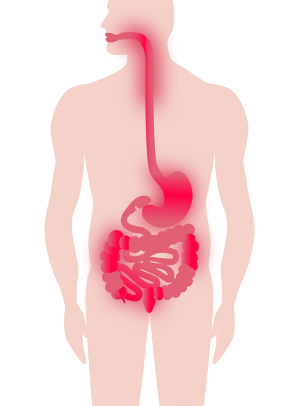
In order to understand Crohn’s disease and ulcerative colitis, it is first helpful to understand the anatomy and function of the healthy gastrointestinal (GI) tract. Below is a medical illustration of the GI tract. When you eat, food travels through the GI tract in the following order:
Mouth [ 1 ]
Esophagus [ 2 ] (tube that connects the mouth to the stomach)
Stomach [ 3 ] (food is mixed with stomach acid and enzymes to break down the material into smaller pieces called chyme)
Small Bowel [ 4 ] (or the ‘Small Intestine’) is made up of three sections: Duodenum [ 7 ] (about 8 cm in length); Jejunum [ 8 ] (around 3 metres long); and Ileum [ 9 ] (about 3 metres in length).
The functions of the small bowel are to digest your food and absorb the nutrients. In particular, the jejunum and ileum are the organs responsible for absorbing nutrients from your food. Without the small bowel, we would not be able to convert food into useable nutrition.
Ileocecal Valve [ 5 ] (regulates the amount of material passed from the small bowel to the large bowel and prevents “dumping” all at once)
Large Bowel [ 6 ] (also called the Large Intestine or the Colon). The colon is much wider in diameter than the small bowel and is approximately 1.5 metres long. The different sections of the colon are identified as the:
- Cecum [ 10 ] and appendix [ 11 ]
- Ascending colon
- Hepatic flexure (a bend in the gut at close to the location of the liver)
- Transverse colon
- Splenic flexure (another bend located near the spleen)
- Descending colon
- Sigmoid colon
- Rectum [ 12 ]
- Anus [ 13 ]
The main functions of the colon are to extract water and salt from stool, and store it until it can be expelled via the anus.
Bowel movements are an entirely different matter for someone with Crohn’s or colitis. Individuals with these diseases face some very real challenges related to feelings of urgency, diarrhea, and bloody stool.
WHAT IS CROHN’S DISEASE
Crohn’s disease is named after the doctor who first described it in 1932 (also known as ‘Crohn disease’).
Inflammation from Crohn’s can strike anywhere in the gastrointestinal (GI) tract, from mouth to anus, but is usually located in the lower part of the small bowel and the upper colon.
Patches of inflammation are interspersed between healthy portions of the gut, and can penetrate the intestinal layers from inner to outer lining.
Crohn’s can also affect the mesentery, which is the network of tissue that holds the small bowel to the abdomen and contains the main intestinal blood vessels and lymph glands.
WHAT IS ULCERATIVE COLITIS
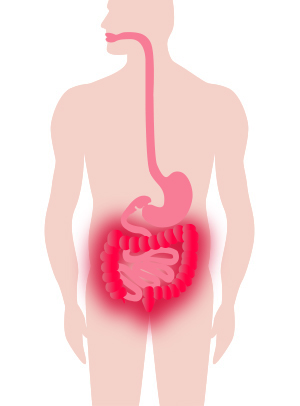
Ulcerative colitis is more localized in nature than Crohn’s disease. Typically, the disease affects the colon (large intestine) including the rectum and anus, and only invades (inflames) the inner lining of bowel tissue.
It almost always starts at the rectum, extending upwards in a continuous manner through the colon. Colitis can be controlled with medication and in severe cases can even be treated through the surgical removal of the entire large intestine.
WHAT IS INDETERMINATE COLITIS:
Indeterminate colitis is a term used when it is unclear if the inflammation is due to Crohn’s disease or ulcerative colitis.
SYMPTOMS OF CROHN’S DISEASE AND ULCERATIVE COLITIS
Crohn’s disease and ulcerative colitis are (lifelong) diseases. People with these diseases experience acute periods of active symptoms (active disease or flare), and other times when their symptoms are absent (remission).
Symptoms can include abdominal pain and cramping; severe diarreha; rectal bleeding; blood in stool; weight loss and diminished appetite.
Visit our Signs and Symptoms page for more information.
COMPARING CROHN’S DISEASE AND ULCERATIVE COLITIS
There are similarities and differences between Crohn’s disease and ulcerative colitis. We’ve already described above how Crohn’s disease and ulcerative colitis involve different areas of the gastrointestinal tract.
Other characteristics of Crohn’s disease and ulcerative colitis that may differ include: symptoms; the effect of surgery; treatment options; complications or extra-intestinal manifestations; and impact of smoking.
These characteristics are summarized in the table below:
| Crohn’s Disease | Ulcerative Colitis | |
|---|---|---|
| Occurrence | More females than males All ages, peak onset 15-35 years |
Similar for females and males All ages, usual onset 15-45 years |
| Symptoms | Diarrhea, fever, sores in the mouth and around the anus, abdominal pain and cramps, anemia, fatigue, loss of appetite, weight loss | Bloody diarrhea, mild fever, abdominal pain and cramps, anemia, fatigue, loss of appetite, weight loss |
| Terminal ileum involvement | Common | Never |
| Colon involvement | Common | Always |
| Rectum involvement | Common | Always |
| Peri-anal disease | Common | Never |
| Distribution of disease | Patchy areas of inflammation | Continuous areas of inflammation but can be patchy once treated |
| Endoscopic findings | Deep and snake-like ulcers | Diffuse ulceration |
| Depth of inflammation | May be transmural, extending through the entire thickness of the wall of an organ or cavity deep into tissues | Shallow, mucosal |
| Fistulas between organs | Common | Never |
| Stenosis | Common | Never |
| Granulomas on biopsy | Common | Never |
| Effect of surgery | Often return following removal of affected parts. Decreased likelihood of pregnancy. | Usually cured by removal of colon (colectomy). Decreased likelihood of pregnancy after ileoanal pouch. |
| Treatment options | Drug treatment (corticosteroids, immune modifiers, biologic therapies). Exclusive formula diet in children. Surgery (repair fistulas, remove obstruction, resection, and anastomosis). | Drug treatment (5-aminosalicylates, sulfasalazine, corticosteroids, immune modifiers, biologic therapies). Surgery (rectum/colon removal) with creation of an internal pouch (ileoanal pouch). |
| Cure | No existing cures. Maintenance therapy is used to reduce the chance of relapse. | Through colectomy only. Maintenance therapy is used to reduce the chance of relapse. |
| Bowel complications | Blockage of intestine due to swelling or formation of scar tissue. Abscesses, sores, or fistulas. Malnutrition. Colon cancer. | Bleeding from ulcerations. Perforation (rupture) of the bowel. Malnutrition. Colon cancer. |
| Extra-intestinal disease | Osteoporosis. Liver inflammation (primary sclerosing cholangitis). Blood clots. Pain and swelling in the joints (arthritis). Growth failure (in children). Mental Illness. | Liver inflammation (primary sclerosing cholangitis). Blood clots. Eye inflammation (iritis). Pain and swelling in the joints (arthritis). Mental illness. |
| Smoking | Higher risk of acquiring for smokers | Higher risk of acquiring for ex-smokers |
| Mortality risk | Increased risk of colorectal cancer and overall mortality. Increased risk of lymphoma and skin cancer (due to treatments). | Increased risk of colorectal cancer. Uncertain change in mortality risk. Increased risk of lymphoma and skin cancer (due to treatments). |
Image reference. Impact of Inflammatory Bowel Disease in Canada. 2018.
Information taken from https://crohnsandcolitis.ca/About-Crohn-s-Colitis/What-are-Crohns-and-Colitis
Discussion (0)
There are no comments for this doc yet.
Comment posting has been disabled on this doc.